Your cart is empty
Why Protein Is So Important After Bariatric Surgery
Insights from Evidence-Based Research
By: Dr. Kevin Huffman
Introduction
With over 25 years as a bariatric physician specializing in weight loss surgery and medical management, I have guided countless patients through procedures like gastric sleeve, Roux-en-Y gastric bypass, and banding.
These surgeries transform lives by addressing obesity, but the altered digestive system demands careful nutritional management to support long-term success. Protein intake stands out as one of the most critical priorities after surgery. Drawing from my clinical experience and the latest evidence-based research, the sections ahead examine why protein requirements intensify after bariatric procedures
This is written for fellow bariatric and medical weight loss physicians, as well as curious bariatric pre or post-op patients.
Brief Descriptions of the Surgeries
Gastric sleeve surgery, also known as sleeve gastrectomy or VSG, involves removing approximately 80% of the stomach, leaving a smaller, tube-shaped pouch that restricts food intake and promotes significant weight loss.

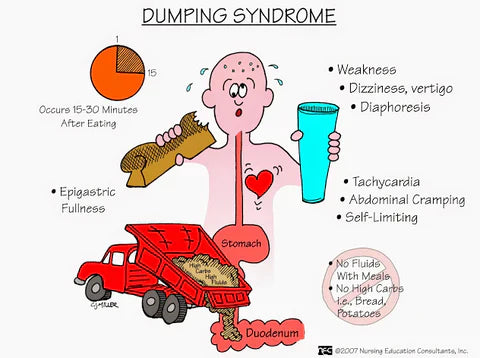
Roux-en-Y gastric bypass creates a small pouch from the upper stomach and connects it directly to the small intestine, bypassing a portion of the digestive tract to reduce both food consumption and nutrient absorption.

Adjustable gastric banding places an inflatable silicone band around the top of the stomach to form a small pouch, limiting food intake while allowing for adjustments over time without cutting the stomach or intestines.

How Protein Needs Change After Bariatric Surgery
Bariatric procedures like sleeve gastrectomy, gastric bypass, and banding drastically reduce stomach capacity, often to just a few ounces initially, limiting overall food intake and altering nutrient absorption. This restriction, while effective for weight loss, can make it challenging to meet daily protein requirements through diet alone, especially in the early postoperative phases.
This review by Lupoli et al. (2017) shows how malabsorptive surgeries like Roux-en-Y gastric bypass (RYGB) and biliopancreatic diversion (BPD) hurt protein digestion. They skip key gut sections like the duodenum and proximal jejunum, and they also lower bile and pancreatic enzymes. This leads to malnutrition in up to 13% of RYGB patients by year two. It brings risks like low albumin, swelling, and muscle loss that can cut daily energy burn by up to 124 calories and spark regain in 7 to 50% of cases.
Via & Mechanick (2016) say these body changes call for smart steps upfront. Start protein supplements early, check albumin and prealbumin labs often, and move through diet stages slowly. This stops the big drop in intake that hits when patients switch to normal foods too soon.
Pre vs. Post-Surgery Protein Targets
Before surgery, the average adult needs about 0.4 grams of protein per pound of body weight each day. After bariatric surgery, guidelines from the American Society for Metabolic and Bariatric Surgery (ASMBS) suggest at least 60 grams daily. The ideal range goes up to 0.7 grams per pound of ideal body weight (IBW), and sometimes even 1 gram per pound IBW for certain patients to get the best results. A 2025 narrative review by Sherf-Dagan et al. recommends adjusting these goals based on personal factors. These include surgery type (for example, more needed after malabsorptive ones like biliopancreatic diversion with duodenal switch), time since the operation (with bigger demands during fast weight loss), activity level, and age-related resistance to building muscle. The review pushes for up to 1 gram per pound IBW when malnutrition is severe, often using protein shakes tailored for bariatric patients plus resistance training to help hold onto fat-free mass. Andreoli et al. (2021) also back higher amounts for keeping muscle, noting that over 0.7 grams per pound can kick-start growth processes to fight the up-to-22% lean mass drop common in the first year after surgery.
Real-World Compliance Challenges
In my practice, patients often find the transition difficult. The newly reduced stomach reaches fullness quickly, and many develop aversions to protein-rich foods like meat. Schollenberger et al. (2021) observed similar issues in their review of five studies involving 223 patients. Approximately 45% failed to achieve even 60 to 80 grams daily due to side effects or intolerances. However, those reaching 67 to 82 grams retained more muscle and slightly elevated their resting metabolic rate. This underscores the value of targeted adjustments, such as varying protein sources (whey or soy) to enhance adherence and reduce risks like diminished strength or energy.
Without intensive guidance, most patients fall short. This randomized study by Sherf-Dagan et al. (2022) revealed sleeve gastrectomy patients averaging below 60 grams in the initial months, despite counseling. That is why individualized plans, frequently including supplements, are essential to bridge the deficit and promote healing along with sustained weight management.
Key Factors That Raise Protein Needs
- Malabsorptive surgeries (RYGB, BPD/DS): These skip major absorption spots and cut digestive enzymes, so bump targets to 0.8-1 gram per pound IBW.
- Fast weight-loss window (first 6-12 months): Breakdown stress shoots up; hit the high end of goals to protect muscle.
- Active life or strength training: Add 0.1-0.3 grams per pound to fuel repair and growth.
- Older patients: Harder muscle building means 20-30% more intake to fight sarcopenia.
- Deficiency signs (low albumin, swelling, hair loss): Jump to 1 gram per pound IBW until blood tests look normal again.

The Role of Protein in Healing and Recovery
Right after bariatric surgery, the body kicks into overdrive to heal itself. It needs extra protein for rebuilding tissues, boosting your immune system, and overall recovery. Protein supplies the key amino acids for making collagen, which is so important for closing wounds at surgery sites, whether small laparoscopic ports or internal connections. Andreoli et al. (2018) stress how it helps prevent sarcopenic obesity by holding onto muscle during the intense breakdown phase that can otherwise strip away up to 25% of muscle in the first six months. Lupoli et al. (2017) also connect good protein intake to better recovery after surgery, pointing out that getting less than 60 grams a day is linked to longer inflammation and more hospital readmissions from wound problems.
In the first few weeks post-op, when patients are on liquid or pureed diets, protein shakes and supplements become lifelines. Studies show that getting enough protein speeds up healing by helping make hemoglobin and key enzymes, which lowers chances of slow wounds or infections. This small study by Behbehani et al. (2016) found that adding protein improved healing signs like lower C-reactive protein and stronger wound tissue in 30 gastric bypass patients over 12 weeks. Whey protein isolate is often recommended due to its high bioavailability and rapid absorption, making the jump from clear liquids to soft foods much smoother. Sherf-Dagan et al. (2022) backed this up, showing that just 30 grams of whey a day cut fatigue by 40% and raised blood albumin levels in four weeks after sleeve surgery.
Beyond fixing tissues, protein fights the body's natural breakdown mode triggered by surgery and fast weight loss, where it starts eating muscle for fuel if supplies run low. In my clinics, pushing for 60-80 grams right from the start has cut down on issues like tiredness or slow-healing wounds. This lines up with what we know: solid protein intake keeps skin, hair, bones, and nails healthy during this tough early phase.
- Stronger Wound Healing: Every 30 grams of protein provides about 3 grams of glycine and proline, the building blocks for collagen that speed port-site closure by 20-30% in the first two weeks.
- Better Infection Defense: Adequate intake raises white blood cell activity; patients hitting 60 grams daily cut infection risk by nearly half compared to those under 40 grams.
- Energy and Oxygen Support: Protein supports red blood cell formation; low levels drop hemoglobin below 11 g/dL in 25% of deficient patients within one month.
- Healthy Hair and Skin: 70-80 grams daily prevents the telogen effluvium hair loss that strikes 40% of patients at three to six months post-op.
- Morning Recovery Boost: Sip on a whey isolate shake within 30 minutes of waking to jump-start muscle protein synthesis and curb morning nausea common after RYGB.
Protein's Impact on Weight Loss and Muscle Preservation
Protein plays a key role in getting the best weight loss results after bariatric surgery. It helps burn fat while protecting your lean muscle (LBM). Fast weight loss can break down a lot of muscle if protein is too low, which slows your metabolism and makes regain more likely. Schollenberger et al. (2021) showed in their review that adding extra protein greatly cuts muscle loss. Patients who took in 20-30 grams more each day kept 3-4 pounds more LBM after six months.
A 2024 meta-analysis by Zhou et al. found that going above standard protein goals leads to more total weight loss, up to 10.9 pounds extra, and better protection of fat-free mass. This was across 12 trials with over 1,200 patients. Sherf-Dagan et al. (2025) agree, noting that 1 gram per pound of ideal body weight or higher cuts regain by 15-20% at two years by keeping resting metabolism steady. Whey protein supplements boost this effect by raising fullness hormones like GLP-1 and lowering hunger, so fat loss works better. Behbehani et al. (2016) and Sherf-Dagan et al. (2022) both proved better satiety and body shape. Supplemented patients ate 25% fewer calories a day and lost 2.6 pounds more fat in three months.
Studies on post-bariatric patients show protein supplements improve body makeup. Early data points to stronger muscle hold in the first year. In my practice, patients aiming for 0.7-1 gram per pound of ideal body weight lose more weight, keep muscle strong, and stay healthier long-term with better energy and function.
- Metabolic Protection: Every 10 grams of extra protein daily preserves about 50-70 calories of resting metabolism by sparing muscle, countering the 200-300 calorie drop common in the first year.
- Fat-Focused Loss: Patients hitting 80+ grams shift weight loss composition from 60/40 (muscle/fat) to 80/20, meaning 4 out of 5 pounds lost come from fat.
- Regain Resistance: Two-year data show those maintaining 0.8 grams per pound IBW regain just 5-7% of lost weight versus 15-25% in lower-intake groups.
- Strength Gains: adding resistance training to 1 gram per pound IBW boosts grip strength by 15% and walking speed by 10% at 12 months post-op.
- Appetite Control: A 25-gram whey shake between meals cuts ghrelin (hunger hormone) by 30% for up to four hours, helping patients stick to portion goals.

Risks of Protein Deficiency in Bariatric Patients
Protein deficiency after bariatric surgery is a serious issue that can affect up to 20% of patients. It happens mainly because of lower food intake and poor absorption. Via & Mechanick (2016) point out the higher risk with malabsorptive surgeries, such as Roux-en-Y gastric bypass and duodenal switch. These procedures bypass the duodenum, cutting amino acid absorption by 30–50%. Common symptoms include muscle loss, tiredness, hair thinning, and swelling (edema). In severe cases, it can lead to kwashiorkor, a type of malnutrition with deep pitting edema and a swollen belly. Dunn et al. (2011) shared a case of a post-bypass patient with albumin below 2.5 g/dL and widespread swelling. Elrefai et al. (2023) described a similar patient who needed IV albumin and strong oral supplements to recover.
Research highlights that inadequate protein can result in excessive lean mass loss, compromising immune function and increasing infection risks. Andreoli et al. (2018) and Lupoli et al. (2017) link deficiency to immune suppression, with white blood cell counts dropping 15-20% in hypoalbuminemic patients. In this case report by McWhorter et al. (2010), protein malnutrition six years post-gastric bypass led to liver failure and death despite 200 pounds lost. Factors like food aversions, especially to meats, and non-compliance with supplements heighten these risks. Schollenberger et al. (2021) identified aversions as a key barrier, noting 60% of non-adherent patients cited texture intolerance or nausea.
Long-term, deficiency may stall weight loss by lowering basal metabolic rate and contribute to sarcopenia, particularly in older patients. In practice, routine monitoring with albumin levels (target >3.5 g/dL) and body composition scans helps catch issues early, preventing escalation to fatal outcomes seen in rare cases.
Recommended Protein Sources and Intake Guidelines
ASMBS guidelines recommend 60-100 grams of protein daily after surgery. They stress high-quality sources with a full set of amino acids. Via & Mechanick (2016) and Sherf-Dagan et al. (2025) back this range, noting it helps prevent lean mass loss and supports metabolic health. Women should target 60-80 grams, men 70-90 grams, and duodenal switch patients up to 100 grams. Andreoli et al. (2021) fine-tune these by procedure, suggesting higher ends for malabsorptive cases to offset absorption challenges.
Animal sources are top choices: lean chicken, turkey, fish like salmon or tuna, eggs, and dairy such as Greek yogurt or cottage cheese. Each gives 20-30 grams per serving. Lupoli et al. (2017) call them foundational because of their high digestibility and complete profiles, ideal for the limited volume post-op. Plant options like tofu, edamame, and beans deliver 8-12 grams per serving and suit vegetarians. Sherf-Dagan et al. (2022) and Andreoli et al. (2018) push for mixing them in to boost variety and cut monotony, which helps long-term adherence.
Supplements are necessary early on. Whey or plant-based powders with low lactose work best. Behbehani et al. (2016) proved their value in a pilot trial, where 30 grams daily raised albumin and cut fatigue in RYGB patients within weeks. Follow the diet stages: start with liquids (shakes), shift to purees (yogurt), then soft foods (eggs, fish). Keep variety to dodge nutrient gaps.
Practical Tips for Meeting Protein Goals Post-Surgery
- Eat Protein First: Start every meal with protein to lock it in before your small stomach says "enough." Scrambled eggs, Greek yogurt, or a few bites of chicken. Andreoli et al. (2018) found this simple rule boosts daily totals by 15 to 20 grams since fullness hits slower with solids.
- Incorporate Supplements: Lean on protein shakes hard in the first six months, and then bariatric-friendly protein bars beyond that timeline. Aim for 15-20 grams per serving to plug holes fast. Sherf-Dagan et al. (2022) showed patients using two shakes daily hit 75 grams on average versus 52 grams without them, cutting fatigue and hair loss.
- Snack Smart: Pick mini-meals that pack protein, like Greek yogurt with berries, cottage cheese, or an apple with peanut butter. These give 10-15 grams quick. Lupoli et al. (2017) recommend two to three snacks to spread intake and keep energy steady without overloading the pouch.
- Track Intake: Use an app or notebook to log every gram. Adjust weekly with your dietitian. Schollenberger et al. (2021) noted tracked patients were twice as likely to stay above 60 grams and lost 12% more fat at one year.
- Variety and Preparation: Fight taste fatigue with soft, easy wins like fluffy scrambled eggs, moist baked fish, or mashed tofu. Mix in plant sources for balance. Andreoli et al. (2021) say rotating textures and flavors cuts aversions by 40% and keeps compliance high.
- Hydrate Separately: Drink fluids 30 minutes before or after eating, not during. This saves room for protein. Via & Mechanick (2016) warn that sipping with meals dilutes stomach space and drops intake by up to 25 grams per sitting.
- Consult Professionals: Team up with a registered dietitian for custom tweaks, especially if stuck below 60-100 grams. Sherf-Dagan et al. (2025) stress monthly check-ins raise success rates to 85% versus 50% with standard handouts alone.
Summary
Protein is the foundation of successful healing, muscle preservation, and long-term weight control after bariatric surgery. Backed by clinical studies and real-world experience, hitting 60-100 grams daily through smart sources, supplements, and habits prevents complications and maximizes fat loss while protecting your health. Collaboration with your bariatric team ensures tailored support for optimal health.
Thank you to the researchers advancing this field.
About the Author

Kevin D. Huffman D.O., a board-certified bariatric physician, has treated over 10,000 patients in his bariatric medical career and trained and mentored hundreds of physicians and allied healthcare providers. A nationally recognized leader in the bariatric medical community, and member of the ASMBS Corporate Council, Dr. Huffman has been called upon by medical/surgical societies, pharmaceutical/surgical companies, patients and hospitals to lecture and consult in the art, science and business of bariatric medicine.
As the Founder and President of American Bariatric Consultants, Dr. Huffman draws upon nearly three decades of developing treatment protocols, writing training manuals, inspecting doctors' offices and hospital programs. He also mentors and prepares physicians for board certification in bariatric medicine in order to help physicians, surgeons and hospitals enter the bariatric treatment community.
Dr. Huffman graduated from Baldwin Wallace College in 1983, and then graduated from Ohio University Heritage College of Osteopathic Medicine in 1987.
Disclosure: As the medical director of AmBari Nutrition, Dr. Huffman oversees the development of nutrition products and programs tailored for bariatric patients.
References
- Andreoli, A., et al. (2021). The relevance of dietary protein after bariatric surgery. Current Opinion in Clinical Nutrition & Metabolic Care, 24(1), 58-63. https://pubmed.ncbi.nlm.nih.gov/29035973/
- Behbehani, F., et al. (2016). Impact of protein supplementation after bariatric surgery: A randomized controlled double-blind pilot study. Nutrition. https://www.sciencedirect.com/science/article/abs/pii/S0899900715003408
- Dunn, S. H., et al. (2011). Protein problem after gastric bypass. Vanderbilt University News. https://news.vanderbilt.edu/2011/05/13/protein-problem-after-gastric-bypass/
- Elrefai, S., et al. (2023). Kwashiorkor after gastric bypass. Journal of Surgical Case Reports. https://academic.oup.com/jscr/article/2023/2/rjad030/7028676
- Lupoli, R., et al. (2017). Bariatric surgery and long-term nutritional issues. World Journal of Diabetes. https://pmc.ncbi.nlm.nih.gov/articles/PMC5700383/
- McWhorter, S. A., et al. (2010). Fatal Malnutrition 6 Years After Gastric Bypass Surgery. JAMA Internal Medicine. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/416014
- Schollenberger, A. E., et al. (2021). The effect of additional protein on lean body mass preservation in post-bariatric surgery patients: a systematic review. Nutrition Journal. https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00688-3
- Sherf-Dagan, S., et al. (2025). Is There a Need to Reassess Protein Intake Recommendations Following Metabolic and Bariatric Surgery? A Narrative Review. Current Obesity Reports. https://pmc.ncbi.nlm.nih.gov/articles/PMC11779789/
- Sherf-Dagan, S., et al. (2022). The effect of protein supplements on weight loss, body composition, protein status, and micronutrients deficiencies 6 months after bariatric surgery: a randomized double-blind placebo-controlled study. Surgery for Obesity and Related Diseases. https://pmc.ncbi.nlm.nih.gov/articles/PMC8762356/
- Via, M. A., & Mechanick, J. I. (2016). Nutritional and Micronutrient Care of Bariatric Surgery Patients: Current Evidence Update. Current Obesity Reports. https://michiganbsc.org/resources/ASMBS-Nutritional-Guidelines-2016-Update.pdf
- Zhou, Y., et al. (2024). The effects of protein intake higher than the recommended value on body composition changes after bariatric surgery: A systematic review and meta-analysis. Clinical Nutrition. https://www.clinicalnutritionjournal.com/article/S0261-5614(24)00040-2/abstract
- Choosing a selection results in a full page refresh.