Your cart is empty

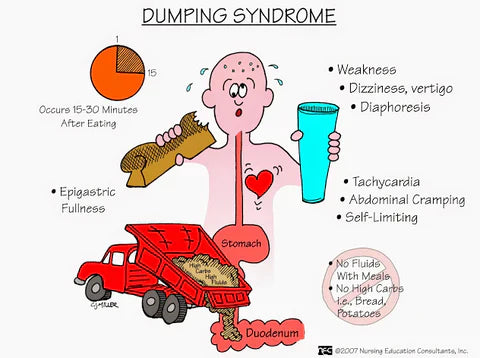
Complete Guide to Dumping Syndrome
Understanding, Managing, and Preventing Dumping Syndrome After Bariatric Surgery
🧭 Quick Navigation
What is Dumping Syndrome?
Dumping Syndrome Definition
Dumping syndrome, also called rapid gastric emptying, is a condition where food moves too quickly from the stomach into the small intestine without being properly digested. This rapid transit occurs when the normal stomach function that regulates food passage is altered, most commonly after gastric or bariatric surgery. The uncontrolled movement of undigested food causes a range of uncomfortable symptoms that can significantly impact quality of life.
Dumping Syndrome by the Numbers
🔄 How Normal Digestion Works
- Food enters stomach and mixes with acid
- Stomach acts as temporary storage reservoir
- Pyloric valve controls release rate
- Small amounts gradually enter intestine
- Proper digestion and absorption occur
- Blood sugar remains stable
⚡ What Happens in Dumping Syndrome
- Food bypasses normal stomach processing
- Large amounts rapidly enter intestine
- Intestine becomes overwhelmed
- Fluid shifts from blood to intestine
- Hormones released in excess
- Blood sugar spikes then crashes
Dumping syndrome is essentially a mismatch between what your altered digestive system can handle and what you're asking it to process. Understanding this fundamental mechanism is the first step toward successful management. It's not just about avoiding certain foods - it's about working with your new anatomy in a way that promotes optimal health and prevents uncomfortable episodes.
Dr. Kevin Huffman, Bariatric Physician
Early vs Late Dumping Syndrome
Early Dumping Syndrome (10-30 minutes after eating)
Mechanism: Rapid movement of hyperosmolar (concentrated) food into the small intestine causes fluid to shift from blood vessels into the intestinal lumen. This creates intestinal distension and triggers the release of gut hormones.
Primary Trigger: High-sugar foods, large portions, or eating too quickly
Key Feature: Gastrointestinal and cardiovascular symptoms occur together
Late Dumping Syndrome (1-3 hours after eating)
Mechanism: Also called reactive hypoglycemia, this occurs when rapid sugar absorption triggers excessive insulin release, causing blood glucose to plummet below normal levels.
Primary Trigger: High-carbohydrate meals, especially simple sugars
Key Feature: Hypoglycemic symptoms similar to diabetes medication reactions
| Aspect | Early Dumping | Late Dumping |
|---|---|---|
| Timing | 10-30 minutes after eating | 1-3 hours after eating |
| Primary Cause | Fluid shifts and intestinal distension | Reactive hypoglycemia from insulin spike |
| Main Triggers | High-sugar foods, large portions, liquids with meals | Simple carbohydrates, sugary foods, refined sugars |
| Blood Sugar Pattern | May spike initially | Spikes then crashes dangerously low |
| Predominant Symptoms | Nausea, cramping, diarrhea, sweating | Shakiness, confusion, weakness, heart palpitations |
| Management Focus | Portion control, food choices, eating technique | Carbohydrate restriction, blood sugar stabilization |
⚠️ Important Distinction
Many patients experience both early and late dumping syndrome. The symptoms may overlap or occur at different times depending on what and how much you eat. Understanding both types helps you identify triggers and implement appropriate prevention strategies for each situation.
Dumping Syndrome Symptoms
🚨 Early Dumping Symptoms (10-30 min)
Gastrointestinal Symptoms:
- Nausea and vomiting
- Abdominal cramping and pain
- Bloating and feeling of fullness
- Diarrhea (30-60 minutes later)
- Borborygmi (rumbling stomach sounds)
Cardiovascular/Systemic Symptoms:
- Rapid heart rate (tachycardia)
- Sweating and flushing
- Dizziness and lightheadedness
- Feeling faint or weak
- Desire to lie down
🩸 Late Dumping Symptoms (1-3 hours)
Hypoglycemic Symptoms:
- Shakiness and tremors
- Cold sweats
- Rapid or irregular heartbeat
- Anxiety and nervousness
- Confusion and difficulty concentrating
- Weakness and fatigue
- Hunger and food cravings
- Irritability and mood changes
Severe Cases May Include:
- Near-fainting or syncope
- Severe cognitive impairment
- Loss of consciousness (rare)
💡 Symptom Recognition Tips
- Keep a symptom diary: Track what you eat, when symptoms occur, and their severity
- Note timing patterns: Early symptoms happen quickly, late symptoms are delayed
- Identify trigger foods: Most episodes are food-related and preventable
- Monitor blood sugar: Use a glucometer during late dumping episodes if you have diabetes
- Rate severity: Mild symptoms may be manageable, severe symptoms require medical attention
🚨 When Dumping Syndrome Becomes Dangerous
While dumping syndrome is typically not life-threatening, severe cases can lead to dehydration from persistent diarrhea, significant weight loss from food avoidance, malnutrition, and dangerous hypoglycemic episodes. If you experience repeated severe symptoms, persistent weight loss, or blood sugar drops below 50 mg/dL, seek immediate medical attention.
Causes and Risk Factors
⚕️ Surgical Causes
Most Common:
- Gastric bypass (Roux-en-Y) - highest risk
- Sleeve gastrectomy
- Gastric band (less common)
- Duodenal switch
Other Surgeries:
- Gastrectomy (stomach removal)
- Esophagectomy
- Fundoplication (GERD surgery)
- Vagotomy
- Pyloroplasty
🍽️ Dietary Triggers
High-Risk Foods:
- Simple sugars: Candy, cookies, cake
- Sugary drinks: Soda, juice, sports drinks
- Refined carbs: White bread, pasta, rice
- High-sugar fruits: Grapes, watermelon, dried fruits
- Dairy products: Milk, ice cream (lactose)
- Processed foods: High-sugar snacks and desserts
Eating Behaviors:
- Eating too quickly
- Large portion sizes
- Drinking with meals
- Very hot or cold foods
🔍 Medical Risk Factors
Existing Conditions:
- Type 2 diabetes (especially prevalent)
- Gastroparesis
- Peptic ulcer disease
- Zollinger-Ellison syndrome
- Cyclic vomiting syndrome
Individual Factors:
- Surgery type and extent
- Individual anatomy
- Healing patterns
- Compliance with post-op diet
- Pre-existing diabetes
⏰ Timeline Factors
When It Develops:
- Can occur immediately post-surgery
- May develop months or years later
- Often emerges when transitioning to solid foods
- Can worsen with dietary compliance lapses
- May improve over time with proper management
🎯 Why Gastric Bypass Has Highest Risk
Roux-en-Y gastric bypass carries the highest risk of dumping syndrome because it completely bypasses the stomach's normal function. The small stomach pouch connects directly to the small intestine, eliminating the pyloric valve that normally controls food release. This creates a direct pathway for undigested food to rapidly enter the intestine, triggering the cascade of symptoms. Additionally, the shortened digestive tract affects hormone release patterns, contributing to both early and late dumping symptoms.
Dumping Syndrome and Diabetes
⚠️ Critical Information for Diabetic Patients
If you have diabetes, dumping syndrome requires special attention. Late dumping syndrome can cause dangerous hypoglycemic episodes that may be mistaken for diabetes medication reactions. The blood sugar swings can also make diabetes management more challenging, requiring medication adjustments and careful monitoring.
🩸 How Dumping Affects Blood Sugar
The Dangerous Cycle:
- Rapid sugar absorption spikes blood glucose
- Pancreas releases excessive insulin
- Blood sugar crashes to dangerous levels
- Hypoglycemic symptoms occur 1-3 hours later
- May require emergency glucose treatment
💊 Diabetes Management Considerations
- Medication timing: May need adjustment with meal patterns
- Blood sugar monitoring: More frequent testing required
- Hypoglycemia treatment: Keep glucose tablets handy
- Healthcare coordination: Endocrinologist and surgeon communication
- Emergency planning: Family/friends should know signs of severe low blood sugar
| Diabetes Type | Dumping Syndrome Risk | Special Considerations | Management Strategy |
|---|---|---|---|
| Type 2 Diabetes | Higher risk, different mechanism | May have altered insulin response patterns | Focus on carbohydrate restriction, medication adjustment |
| Type 1 Diabetes | Risk varies by individual | Insulin dosing becomes more complex | Careful insulin timing, frequent monitoring |
| Pre-diabetes | May develop during weight loss | Could worsen glucose tolerance temporarily | Lifestyle modifications, monitoring for progression |
| Gestational Diabetes History | Monitor for diabetes development | Hormonal changes post-surgery | Regular screening, dietary vigilance |
💡 Blood Sugar Management Tips
- Test frequently: Check blood sugar before meals and 1-3 hours after
- Recognize patterns: Learn your personal trigger foods and timing
- Carry supplies: Always have glucose tablets or gel available
- Wear medical ID: Identify yourself as having both diabetes and dumping syndrome
- Emergency contacts: Ensure family knows how to respond to severe hypoglycemia
- Regular check-ups: Monitor A1C and adjust medications as needed
Diabetic patients with dumping syndrome face a unique challenge. The rapid blood sugar fluctuations can make diabetes management feel like you're constantly chasing your glucose levels. The key is prevention through strict dietary adherence and working closely with both your bariatric team and endocrinologist to optimize your medication regimen for your new digestive anatomy.
Dr. Kevin Huffman, Bariatric Physician specializing in post-bariatric care
Foods to Avoid and Foods to Embrace
❌ Foods That Trigger Dumping Syndrome
High-Sugar Foods:
- Candy, chocolates, cookies
- Cakes, pastries, donuts
- Ice cream, frozen yogurt
- Sugary cereals
- Honey, syrup, jam
Sugary Beverages:
- Regular soda and soft drinks
- Fruit juices (even 100% juice)
- Sports drinks and energy drinks
- Sweetened coffee drinks
- Milkshakes and smoothies with added sugar
Refined Carbohydrates:
- White bread, white rice
- Regular pasta
- Instant mashed potatoes
- Crackers and pretzels
- Processed breakfast cereals
High-Sugar Fruits:
- Watermelon, grapes
- Dried fruits (raisins, dates)
- Canned fruits in syrup
- Fruit concentrates
✅ Safe Foods for Dumping Syndrome
Lean Proteins:
- Chicken breast, turkey
- Fish and seafood
- Eggs and egg whites
- Lean beef and pork
- Tofu and tempeh
- Greek yogurt (unsweetened)
Complex Carbohydrates:
- Quinoa, brown rice
- Sweet potatoes
- Oatmeal (steel-cut)
- Whole grain breads (small amounts)
- Beans and lentils
Low-Sugar Vegetables:
- Leafy greens (spinach, kale)
- Broccoli, cauliflower
- Bell peppers, zucchini
- Asparagus, green beans
- Tomatoes, cucumbers
Healthy Fats:
- Avocado
- Nuts and seeds (small portions)
- Olive oil
- Fatty fish (salmon, mackerel)
⚠️ Foods to Eat With Caution
Moderate Sugar Content:
- Fresh fruits: Berries, apples (small portions)
- Dairy: Plain milk, cheese (watch lactose)
- Starchy vegetables: Corn, peas, carrots
Individual Tolerance Varies:
- Whole grain products: Start small, monitor response
- Natural sweeteners: Stevia, monk fruit (generally safe)
- Sugar alcohols: May cause digestive upset
🥤 Beverage Guidelines
Safe Options:
- Water (primary choice)
- Unsweetened tea and coffee
- Sugar-free beverages
- Bone broth
- Bariatric protein shakes (bariatric-specific)
Timing Rules:
- No liquids 30 minutes before meals
- No liquids during meals
- Wait 30-60 minutes after eating
- Sip slowly when drinking
💡 Smart Shopping and Meal Planning Tips
- Read nutrition labels: Look for sugar content and serving sizes
- Shop the perimeter: Focus on fresh, whole foods
- Meal prep basics: Prepare safe proteins and vegetables in advance
- Emergency foods: Keep suitable snacks available for busy days
- Restaurant strategies: Research menus ahead, ask about ingredients
- Portion control tools: Use smaller plates and measuring tools
🎯 The 5-5-15 Rule for Dumping Prevention
5 grams of sugar maximum per serving to prevent triggering
5 minutes minimum eating time for proper digestion
15 grams of protein minimum at each meal for stability
This simple rule helps prevent most dumping episodes while ensuring adequate nutrition!
Proven Management Strategies
🍽️ Dietary Management
Meal Structure:
- Eat 6 small meals daily instead of 3 large ones
- Chew food thoroughly (20-30 chews per bite)
- Eat slowly - take 20-30 minutes per meal
- Stop eating when satisfied, not full
- Protein first at every meal
Portion Control:
- Use measuring tools initially
- Start with smaller portions
- Listen to satiety signals
- Avoid eating past comfort
💧 Fluid Management
Timing Rules:
- No fluids 30 minutes before meals
- No drinking during meals
- Wait 30-60 minutes after eating
- Sip, don't gulp when drinking
- Aim for 64+ ounces of fluid daily
Best Choices:
- Water as primary fluid
- Sugar-free, caffeine-free options
- Herbal teas
- Diluted protein shakes
⏰ Lifestyle Modifications
Eating Environment:
- Minimize distractions: No TV, phones, reading while eating
- Comfortable setting: Sit at table, relaxed atmosphere
- Temperature control: Avoid very hot or cold foods
- Stress management: Calm environment promotes digestion
Post-Meal Strategies:
- Rest position: Lie down for 30 minutes after eating
- Gentle activity: Light walking after resting period
- Monitor symptoms: Track food and symptom patterns
📊 Monitoring and Tracking
Daily Tracking:
- Food diary with symptoms
- Blood sugar levels (if diabetic)
- Hydration status
- Weight and energy levels
- Trigger food identification
Progress Indicators:
- Fewer dumping episodes
- Better energy levels
- Stable weight loss
- Improved quality of life
- Better blood sugar control
Medical Treatment Options When Diet Isn't Enough
| Treatment | How It Works | Effectiveness | Considerations |
|---|---|---|---|
| Octreotide | Slows gastric emptying, reduces hormone release | Effective for severe cases | Injectable medication, potential side effects |
| Acarbose | Slows carbohydrate absorption | Helpful for late dumping syndrome | Oral medication, may cause digestive upset |
| Dietary Fiber Supplements | Slows stomach emptying, stabilizes blood sugar | Mild to moderate benefit | Natural option, requires adequate hydration |
| Revision Surgery | Modifies anatomy to slow food transit | Reserved for severe, refractory cases | Significant procedure, not always successful |
When to See Your Doctor
🚨 Seek Immediate Medical Attention If You Experience:
- Severe hypoglycemia: Blood sugar below 50 mg/dL or loss of consciousness
- Persistent vomiting: Unable to keep fluids down for 24+ hours
- Signs of dehydration: Dizziness, dark urine, extreme thirst
- Chest pain or severe heart palpitations: During or after eating
- Fainting or near-fainting: Especially if recurrent
- Severe abdominal pain: That doesn't resolve with rest
🔴 Red Flag Symptoms
Immediate Concerns:
- Blood sugar consistently below 70 mg/dL
- Multiple severe episodes per week
- Weight loss exceeding 2 pounds per week
- Inability to eat without symptoms
- Symptoms interfering with daily activities
Progressive Worsening:
- Symptoms becoming more frequent
- New foods triggering episodes
- Longer recovery times
- Affecting work or social life
- Developing food phobias
📞 Schedule Regular Follow-up For:
Routine Monitoring:
- Symptom tracking: Review patterns with healthcare team
- Nutritional assessment: Ensure adequate intake despite restrictions
- Weight monitoring: Maintain healthy weight loss pace
- Blood work: Check for deficiencies and metabolic changes
- Medication adjustments: Diabetes medications may need changes
Diabetes Management:
- A1C monitoring every 3-6 months
- Blood pressure checks
- Kidney function tests
- Eye and foot exams
💡 What to Expect at Medical Visits
Assessment Tools:
- Dumping Symptom Rating Scale
- Food and symptom diary review
- Blood glucose tolerance testing
- Nutritional status evaluation
- Quality of life assessment
Potential Tests:
- Oral glucose tolerance test
- Gastric emptying study
- Upper endoscopy
- Comprehensive metabolic panel
- Vitamin and mineral levels
👥 Healthcare Team Coordination
Key Team Members:
- Bariatric surgeon
- Registered dietitian
- Endocrinologist (if diabetic)
- Primary care physician
- Mental health counselor
Communication Strategy:
- Share symptom logs with all providers
- Coordinate medication changes
- Regular team meetings or communication
- Clear emergency contact plan
- Updated medical records access
💡 Preparing for Your Medical Appointments
- Bring detailed records: Food diary, symptom log, blood sugar readings
- List all medications: Include supplements and over-the-counter items
- Prepare questions: Write down concerns and specific questions beforehand
- Describe severity: Rate symptoms on a scale of 1-10
- Timeline documentation: When symptoms started, frequency, triggers
- Bring support: Family member or friend can help advocate and remember information
Frequently Asked Questions
How long does dumping syndrome last after bariatric surgery?
Most cases improve significantly within 3-12 months with proper dietary management. Early dumping syndrome often resolves within 3 months, while late dumping may take 12-18 months to fully resolve. However, some patients may experience occasional episodes long-term, especially if they don't follow dietary guidelines. The key is consistent adherence to eating guidelines and working with your healthcare team.
Can I prevent dumping syndrome completely?
While you can't completely prevent all episodes, proper dietary management prevents 90%+ of dumping syndrome episodes. Following the guidelines of eating small portions, avoiding high-sugar foods, chewing thoroughly, and separating liquids from meals significantly reduces your risk. Most patients learn to manage their condition effectively through lifestyle modifications.
Is dumping syndrome dangerous or life-threatening?
Dumping syndrome is typically not life-threatening, but severe cases can lead to complications including dangerous hypoglycemia, dehydration, malnutrition, and significant weight loss. If you experience blood sugar drops below 50 mg/dL, persistent vomiting, or symptoms that interfere with daily life, seek medical attention promptly.
What should I do during a dumping syndrome episode?
For early dumping: Stop eating immediately, lie down in a comfortable position, and wait for symptoms to pass (usually 30-60 minutes). Stay hydrated but don't drink large amounts at once. For late dumping: If you recognize hypoglycemic symptoms, consume 15g of fast-acting carbohydrates like glucose tablets, then rest and monitor your blood sugar if possible.
Can dumping syndrome occur years after bariatric surgery?
Yes, dumping syndrome can develop or worsen years after surgery, especially if dietary habits become less strict over time. Some patients experience their first episodes months or even years post-surgery when they begin eating foods they previously avoided. This emphasizes the importance of lifelong adherence to post-bariatric dietary guidelines.
How does dumping syndrome affect diabetes management?
Dumping syndrome can significantly complicate diabetes management by causing unpredictable blood sugar swings. Late dumping syndrome can cause dangerous hypoglycemia that requires emergency treatment. Diabetic patients need more frequent blood sugar monitoring, possible medication adjustments, and close coordination between their bariatric team and endocrinologist.
Are there any medications that help with dumping syndrome?
Several medications can help when dietary changes aren't sufficient. Octreotide (Sandostatin) slows gastric emptying and reduces hormone release but requires injections. Acarbose helps with late dumping by slowing carbohydrate absorption. Fiber supplements like psyllium can also help slow gastric emptying naturally. Always discuss medication options with your healthcare provider.
Can I eat any sweets or desserts with dumping syndrome?
While traditional sweets are major triggers, you may be able to enjoy small amounts of desserts made with sugar substitutes like stevia, monk fruit, or erythritol. Sugar-free options designed for diabetics are often better tolerated. Always start with very small portions and monitor your response. Many patients find that their tolerance improves over time, but high-sugar foods remain risky.
🏆 AmBari Nutrition: Your Partner in Success

Managing dumping syndrome successfully requires the right nutritional tools. AmBari Nutrition's complete line of bariatric foods are designed to support your journey:
- ✅ Protein shakes: Low-sugar, high-protein formulations that don't trigger symptoms
- ✅ Meal replacement bars: Convenient nutrition without the dumping risk
- ✅ Vitamin supplements: Bariatric-specific formulations for optimal absorption
- ✅ Educational resources: Ongoing support for long-term success
Our products are specifically formulated for post-bariatric patients, taking the guesswork out of nutrition while keeping you safe from dumping episodes.
Taking Control of Your Dumping Syndrome
Managing dumping syndrome successfully is absolutely achievable with the right knowledge, tools, and support. By understanding the difference between early and late dumping, identifying your personal triggers, following proven dietary strategies, and working closely with your healthcare team, you can minimize episodes and maintain excellent quality of life. Remember that dumping syndrome is a manageable condition, not a life sentence. With consistency, patience, and the right approach, you can enjoy a full, active life while maintaining your weight loss success. The key is education, preparation, and never hesitating to reach out for support when you need it.
Disclaimer: This guide is for educational purposes only and should not replace professional medical advice. Always consult with your bariatric surgeon, dietitian, and healthcare team before making any changes to your diet or treatment plan. Individual responses to foods and treatments may vary significantly.
Author: Carrie H. Carrie is a passionate health and nutrition writer who transforms complex medical research into accessible, evidence-based content to empower readers to make informed choices about their wellbeing. With a background in science and a dedication to helping others live healthier lives, she provides thoughtful analysis of the latest studies and practical, actionable advice readers can apply to their own lives. |
Reviewed By: Dr. Kevin Huffman Dr. Huffman is an accomplished board-certified bariatric physician with extensive clinical experience and expertise in treating obesity. He has trained countless healthcare providers and founded American Bariatric Consultants to develop highly sought-after protocols, training materials and continuing education used widely by medical societies, hospitals and physicians. Dr. Huffman's impact reaches far beyond direct patient care, as he actively prepares the next generation of physicians to achieve board certification in bariatrics, thereby exponentially expanding access to this vital medical treatment. |
- Choosing a selection results in a full page refresh.